One Weak Password Just Cost a Hospital $4 Million
INTRODUCTION - THE HIDDEN DANGER IN PLAIN SIGHT
A hospital administrator enters the office on a Tuesday morning, with coffee in hand, prepared for another crowded day. After a few hours, the day changes into a nightmare that will put the organization nearly $4 million out of pocket and make a deep cut in the trust of the patients. The reason? A single weak password.
This is not a fantasy. It is one of the tragedies that often happen in healthcare organizations all over the world. The incident that we are addressing where one reckless choice of credentials caused a catastrophic data breach, has turned the corner in the awareness of cybersecurity. It compels us to - albeit reluctantly - accept that in the race to modernize health care, the juggernaut has sometimes overlooked the essentials of digital security.
Healthcare industry digitization has rapidly progressed. Electronic health records, cloud-based systems, telehealth platforms, and interconnected medical devices have all very positively impacted patient care. Nevertheless, this digital transformation has also brought to the table a huge area of vulnerability that cyber criminals are very much interested in and are even willing to fight for it with the easiest methods like getting hold of a weak password reused across multiple systems instead of trying to exploit unpatched vulnerabilities or sophisticated attacks wispy.
THE BREACH - A TIMELINE OF DISASTER
This saga starts off with a hospital employee, who, like many others at that time, chose the easy way out. A very busy and harried shift made this person resort to one of the easiest and weakest passwords - something like "Welcome123" or "Hospital2024" - for multi-system access. It was easy to use, easy to remember, and unfortunately, already compromised during a breach at a completely different organization.
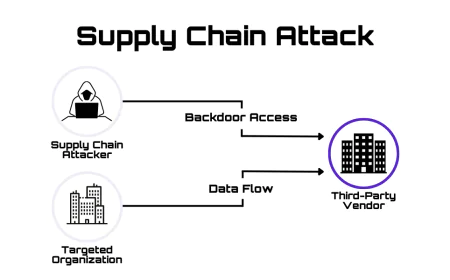
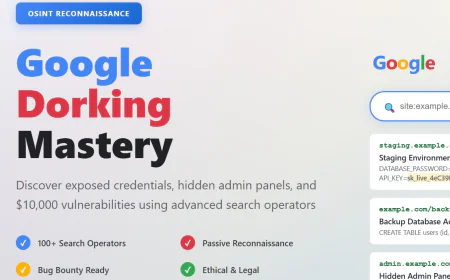
This password was on the dark web where it was recorded in databases that cybercriminals use for credential stuffing attacks. The automated tools ran the password through the hospital’s remote access portal, which was for third-party vendors and administrative access, and the attempt got through. The intruder was already inside.
The situation that followed was a typical one. The invader spent hours systematically going through the network, jumping from one system to another, and raising privileges with each movement. The administrative login details were extracted. The patient databases were found. The records of 200,000 patients with the most sensitive data were accessed and exfiltrated. The attacker even installed ransomware, preventing any access to the critical servers until payment was made.
The hospital's security team required 48 hours to detect the unusual activity. By that time the damage was already very big. The hospital had to make a very difficult decision: either pay the ransom to get access back immediately or refuse and suffer through a long outage. The financial and operational impacts would be significant in both cases.
WHY HOSPITALS ARE PRIME TARGETS?

To figure out the why behind this, it is first necessary to know about the reasons that make cyber criminals so keen on hospitals as their targets.
Healthcare data is priceless beyond measure. A complete medical record along with insurance and personal details can be sold for as much as $250 on the dark web - which is significantly higher than a stolen credit card number that might only bring in a few bucks. This attraction of money leads to well-planned, professional-style attacks on health care providers.
However, there is one more thing that puts hospitals in a vulnerable position: they have to work under exceptional conditions. Unlike the case of regular businesses, hospitals put patients' lives first and nothing else. Security mechanisms that hinder the clinical process are always challenged. The personnel working in hospitals are always busy, poorly paid, and sometimes not well trained in good cybersecurity practices. Financial constraints imply that outdated, unpatched systems continue operating along with the new modern infrastructure. The IT departments are always trying to keep pace with the threats while supporting the crucial life-saving systems that cannot be shut down even for the time required to update them.
Such a condition is a perfect mix to cause the biggest storm possible. There is a huge potential profit for the attackers but the defenses are usually weak and their resources are not enough.
THE ANATOMY OF FAILURE – WHAT WENT WRONG
Security analysts, who were specialists in security, examined the case of this breach, and they found out that there were several failures in a chain reaction that led to the incident—none of these failures were very complicated or hard to prevent.
WEAK PASSWORD PRACTICES
The primary cause was evident, and it was the use of the same passwords along with no multi-factor authentication provided, which was pretty much the same thing as no security at all. The hospital had done nothing to enforce the use of strong passwords or to make employees use different passwords for different systems. If Multi-factor authentication (MFA) had been in place, the attacker would have been blocked right away, even though he had valid credentials.
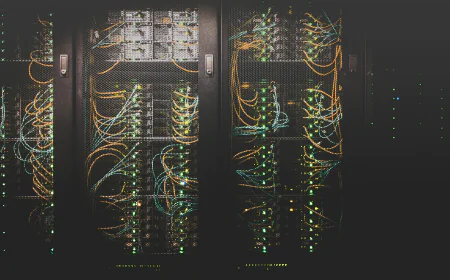
LACK OF NETWORK SEGMENTATION
The attacker was already inside the network and he changed his location to different systems without any restriction. There were no firewalls or access control that restricted the reach of the one credential that was compromised. The database of critical patients was in the same network as the general administrative system with a little separation between them.
OUTDATED SECURITY PATCHES
The analysis showed that some of the critical servers had not been updated for six months and therefore the vulnerabilities were still open. The attackers had exploited these vulnerabilities to gain access and then moved laterally around the network.
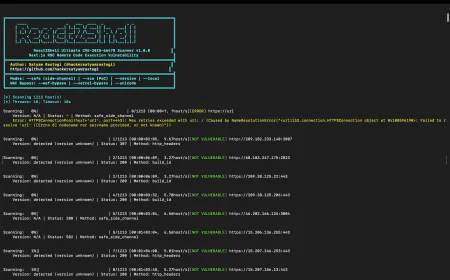
INSUFFICIENT MONITORING
The monitoring tools that the hospital had were not able to detect the lead signals of the breach because they were not properly set up. The hospital was not aware of the abnormal data access, unexpected file transfers, and privilege escalations for almost two days.
Eventually, when the staff did notice something wrong, there was no response playbook for them. The lack of clarity in who should be informed, what to do, and how to contain the compromise led to the waste of precious time.
These were not problems with technology but rather problems of process and prioritization.
UNPACKING THE $4 MILLION COST
The breakdown of the $4 million provides a clearer picture of the incident's huge impact:
SYSTEM RESTORATION AND RECOVERY: $1.2 MILLION
This amount was used for forensic investigation, system restoration, and data recovery. Cybersecurity experts were required to monitor the attack's every step, clean the system of malware, and restore the compromised systems from backups while also confirming data integrity.
LEGAL AND REGULATORY FINES: $800,000
This sum was allocated to covering legal costs and compliance penalties. Healthcare data breaches lead to the compulsory notifications under HIPAA rules, possible state-level breach notification laws, and also may attract regulatory penalties resulting from audits by state attorneys general and the Department of Health and Human Services Office for Civil Rights.
RANSOM PAYMENT: $600,000
This amount was paid for decrypting the hospital's servers and regaining access to critical systems. A lot of hospitals are in a dilemma in such situations—either to pay the criminals or to face prolonged downtime that disrupts patient care.
REPUTATION MANAGEMENT AND PR: $400,000
This was spent on crisis communication, patients' notifications, credit monitoring, and media coverage management. It is costly to gain back the trust of patients after it has been lost.
LOST REVENUE FROM DOWNTIME: $1 MILLION
This was the case for operational disruption. Hospitals canceled elective surgeries; emergency rooms sent patients to other hospitals, and all administration stopped. The overall revenue loss was much larger than the initial breach period because patients started going to other hospitals.
The really bad part of it all is that it does not include the unquantifiable costs like the broken reputation, low staff morale, the nervousness of patients and the loss of opportunities, the main hospital resources were diverted from actual patient care.
THE RIPPLE EFFECT – FINANCIAL LOSS IS ONLY THE TIP OF THE ICEBERG
A direct cost of $4 million is indeed a catastrophe, but the actual influence is felt much wider than the mere numbers on a spreadsheet.
Patient trust vanished in a split second. The precursors of identity theft thousands of patients whose private medical information was leaked, were stressed and anxious. Some changed their providers. Others became more resistant to digital health initiatives, preferring traditional in-person visits where, it seemed, paper records were somehow safer.
Staff morale took a nosedive. Healthcare workers, already under enormous pressure, were blamed for the security breach and yet, at the same time, were dealing with the operational disruption caused by the breach response. A few even left the organization completely.
The hospital's reputation took a hit. The local press was all over the story. Competing hospitals were quietly circling, taking away physicians and staff. Insurance companies increased premiums. Vendor relationships turned sour as third parties began to question the hospital's security posture.
WHY PASSWORD SECURITY MATTERS MORE THAN EVER
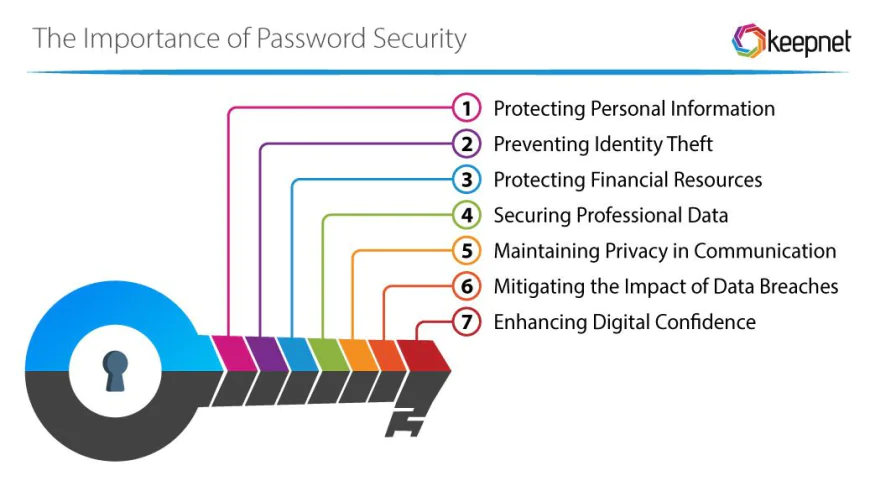
In a time of cutting-edge threats and very up-to-date hackers, it would be a little old-fashioned to concentrate on passwords. However, it still is the password security that constitutes the primary barrier to the flow of attacks besides being the most visible part of security.
The truth is that 81% of confirmed data breaches are due to the use of weak or stolen passwords. Security awareness campaigns had been running for years but failed to improve people's password handling. People still tend to recycle passwords, write them down, tell others about them, and create easily guessable combinations. These actions make the system prone to attacks that are less technical, though much more effective than the supposed technical ones.
The demand for multi-factor authentication should be worldwide, but the fact is that it is still treated as an option in some cases. Properly executed—demanding something you know (password), something you have (phone or security key), or something you are (biometric)—it will automatically eliminate credential-based attacks.
What a paradox! Strong password policies and multi-factor authentication are neither costly nor hard to implement. They are straightforward, reliable, and extremely powerful at the same time. However, they are still often ignored in preference for more attractive solutions or new and advanced technologies.
ENHANCING DEFENSES - PRACTICAL SOLUTIONS
The first step in preventing a $4 million loss is to use a layered strategy that mixes technology, processes, and culture together.
COMPULSORY MULTI-FACTOR AUTHENTICATION
MFA should be implemented on all systems, with remote access portals being the most vulnerable area. This one measure would have halted the attack right away.
STRONG PASSWORD POLICIES
Set minimum password length, specify the different types of characters, and require regular changes. Password reuse across systems should be the biggest prohibition.
NETWORK SEGMENTATION
Admin networks should be separated from clinical systems. Security controls should be present in front of patient data stores to isolate them. Restrict the possibilities of lateral movement.
CONSTANT PATCH MANAGEMENT
A very active security updates schedule should be established. The critical patches should be applied in a few days, not in several months.
SECURITY MONITORING AND ANALYTICS
Real-time tools should be put in place to spot strange access patterns, unauthorized data transfers, and privilege escalations.
REGULAR SECURITY ASSESSMENTS
Keep doing penetration testing and vulnerability scans in order to discover the weak points before the attackers do.
INCIDENT RESPONSE PLANNING
Write down and frequently refresh the methods for breach response that are already detailed. It is important that the whole staff knows their roles and responsibilities.
SECURITY-FIRST CULTURE AT THE CORE - HUMAN FACTOR
No technology could stop breaches by itself. The importance of culture is very high. When employees trust that security is going to be a responsibility shared among all and that it is the main reason for patient safety, their behavior changes.
Security training for awareness should be regularly done and not only be about compliance to annual requirements. It should be done in an engaging way, be relevant to the audience, and be based on real-life scenarios that healthcare workers encounter. Teaching the staff to spot phishing emails, understand social engineering attempts, and alert the authorities about the suspicious activity changes their status from being burdensome to being valuable.
The top management has to make it clear that they are committed to security. When the top executives put cybersecurity on their priority list and make it part of the organizational strategy instead of a cost to the IT department, the message spreads throughout the whole organization. Policies are complied with, best practices are taken up, and a security-conscious culture emerges.
CONCLUSION - MOVING FORWARD
The $4 million password blunder of the hospital should be taken as a clarion call for all healthcare organizations. This was neither a highly advanced country attack nor a zero-day vulnerability. It was a preventable mistake stemming from ignoring the basic principles.
Healthcare institutions are in the business of healing. In the current digital world, safeguarding patient data is as important to that mission as any clinical procedure. A weak password is a wide-open door. An unpatched system is a solicitation. An untrained employee is a potential security risk.
The bright side of the story is that prevention can be achieved. Hospitals, by adopting strong authentication, keeping high-security hygiene, splitting networks, and creating a culture that cherishes security, can significantly lower their breach probability. The expense incurred in these methods is only a small percentage of the loss from a single major breach.
The challenge is not the question of whether healthcare organizations could afford to invest in cybersecurity. It is whether they could afford not to.