Health Insurance Portability and Accountability Act. (HIPAA)
The U.S federal law introduced in year 1996.

Health Insurance Portability and Accountability Act(HIPAA) was established to protect sensitive patient health information. It aims to ensure health insurance portability, reduce healthcare fraud, and establish industry wide standards for healthcare information.
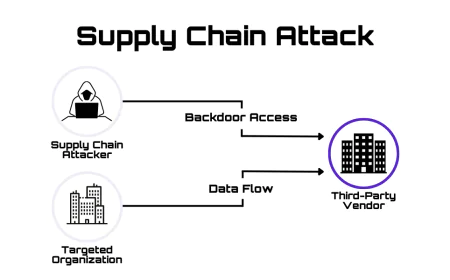
HIPAA applies to Covered Entities (CE) and their Business Associates (BA). Covered entities include healthcare providers, health plans, and healthcare clearinghouses. Business associates are third parties who work with covered entities and handle PHI, such as billing or IT companies.
Key Definations
Protected Health Information (PHI) : Any inforamtion about health status provision of heath care or payment for health care that can be linked to an individual .
ePHI : PHI that is created , stored transmitted or recived electronically.
Breach : Unauthorized acquisition , access , use a disclosure of PHI that compromises security or privacy.
Covered Entity (CE) : Any health plan , health care provider clearinghouse that transmits health information electronically.
Business Associate (BA) : A person or organization that performs or organization that performs activities involving the use or disclosure of PHI on behalf as a cover entity.
BAA : A legal contract between CE and BA outlining how PHI will be handles.
HHS : Health and Human service it is a federal governmnent protecting the heath of Americans.
Key Rules or Core Components of HIPAA
- Privacy Rule : Govern the use and disclosure of Protected Health Information (PHI) and gives patient right over their health records.
- Security Rule : Sets national standards for protecting Electronic Protected Health Information (ePHI) through administration physical and technical safeguards.
- Breach Notification Rule : Required notification of affected individuals , the HHS and sometimes the media following a breach of unsecured PHI .
- Enforcement Rule: Outlines procedures and penalties for HIPAA non-compliance.
Steps to become HIPAA compliant
Step 1 : Conduct a thorough Risk Assessment :
This is fundamental element of HIPAA compliance and must be performed annually. A comprehansive risk assessment identifies potential threats and vulnerabilities to all ePHI.
Step 2 : Implement and Document Safeguards :
Administrative Safeguards are the management policies and procedures that oversee the security of ePHI and conduct of workforce.
- Security Management Process : Develop and implement measures to prevent , detect , contain and correct security violotians.
- Assigne Security Responsibility : Designate a security official to develop and enforce HIPAA policies.
- Workforce Security : Ensure all employees , contractors and volunteers who handle ePHI have the appropriate access levels and clearance for there jobs.
- Security Awareness and Training : Provide regular , documented security training for all workforce members including a plan for disciplinary actions against those who violate policies.
- Contingency Plan : Create data backup ,emergecy mode operation plans to restore last data and continue critical business processes in a emergency.
- Business Associated Agreements (BAAs) : Obtain signed agreements with all third-party vendors who access , stores or transmit ePHI on your behalf.
Physical Safeguards are physical controls that limit and manage access to the area and hardware where ePHI is located.
- Facility access Controls : Implement policies that control physical access to the fecilies.
- Workstation Security : Secure workstations that access ePHI like automatic logoffs or positioning them away from public view.
- Device and Media Controls : Establish policies for secure use , transfer , disposal , and reuse of hardware and electronic media containing ePHI.
- Disposal : Have procedures for the proper and verifiable disposal of ePHI and the media it is stored on.
Technical Safeguards are the technologies and procedures used to secure access to ePHI and monitor its activity.
- Access Controls : Use unique user ID , authentication and encryption to ensure only authorized individual can access ePHI.
- Audit Control : Implement hardware software , or procedural mechanisms to record and examine all activity related to ePHI.
- Integrity Controls : Employ electroinc measures like checksums or digital signatures to ensure that ePHI is not improperly altered or distroyed.
- Transmission Security : Use technical security measures to protect ePHI when it is transmitted over electronic network , such as end-to-end encryption.
Step 3 : Train Employees
Employees are the first line of defence and annual training is required for all staff who handle PHI.
Penalties
- Tire 1 : The violation was due to reasonable issue then fine will be from $141 to $71162 per violation.
- Tire 2 : The violation was due to reasonable issue then fine will be from $1424 to $71162 per violation.
- Tire 3 : The violation was caused by willful neglect but was corrected with in 30 days then fine will be from $14323 to $71162 per violation.
- Tire 4 : The violation was caused by willful neglect and no correction was made within 30 days then the minimum fine will be $71162 per violation.
Importance of HIPAA
- Protects patient privacy by keeping heath information confidential .
- Builds trust netween patients and healtcare providers.